Massachusetts Waiver Amendment Requests Partial Expansion and Closed Formulary
In This Issue
- Massachusetts Waiver Amendment Requests Partial Expansion and Closed Formulary
- Massachusetts Total Healthcare Expenditures: Identifying Cost Drivers
Massachusetts Waiver Amendment Requests Partial Expansion and Closed Formulary
By Patricia M. Boozang, Senior Managing Director, Manatt Health | Deborah Bachrach, Partner, Manatt Health | Mindy Lipson, Senior Manager, Manatt Health | Alexander Dworkowitz, Associate, Manatt Health
On September 8, 2017, Massachusetts submitted a waiver amendment request to the Centers for Medicare & Medicaid Services (CMS) to modify its MassHealth Section 1115 demonstration. The long-standing MassHealth demonstration encompasses the State’s entire Medicaid population and has acted as a major lever for expanding coverage and transforming Massachusetts’ Medicaid payment and delivery landscape. Building on the State’s landmark 2006 health reform (Chapter 58), the demonstration has enabled Massachusetts to achieve the highest rate of insurance in the country, using a combination of expanded Medicaid eligibility, premium assistance for employer-sponsored insurance (ESI) and student health insurance, and Medicaid-funded subsidies for individuals with incomes up to 300% of the federal poverty level (FPL) to purchase coverage on the Connector, the Massachusetts Marketplace. Under the latest demonstration renewal, approved in November 2016, Massachusetts is implementing large-scale payment and delivery system reform to move to a value-based purchasing system of provider-led accountable care organizations (ACOs) operating in partnership with Medicaid managed care organizations and community-based organizations.
Massachusetts’ September application follows a June waiver amendment request, through which Massachusetts seeks to waive the Medicaid requirement to provide nonemergency medical transportation to enrollees receiving the alternative benefit plan (ABP) and eliminate provisional eligibility for adults ages 21 and over whose income is unverified. CMS has not acted on that request to date. Massachusetts is framing its new waiver amendment as a strategy to pursue “additional federal flexibility…for further reforms in MassHealth and the commercial market that support long-term financial sustainability.” The State identifies the following goals:
- "Aligning coverage for non-disabled adults with commercial plans"
- "Adopting widely used commercial tools to obtain lower drug prices and enhanced rebates"
- "Improving care, reducing costs and achieving administrative efficiencies"
- "Supporting access to healthcare for veterans and their families"
Under the newly released application, Massachusetts is the second state after Arkansas seeking approval to implement a “partial expansion,” in which the State would lower its Medicaid eligibility level to 100% FPL, while continuing to receive the Affordable Care Act’s (ACA) enhanced federal medical assistance percentage (FMAP) for members of the expansion group remaining in Medicaid. (As described below, and unlike Arkansas, Massachusetts uses Medicaid dollars at regular FMAP rates to wrap premiums and cost sharing for those individuals with incomes up to 300% FPL who are enrolled in Connector coverage.) In 2012, the Obama administration advised states that the ACA did not authorize enhanced FMAP for partial or phased-in expansions. The Trump administration has not yet indicated whether it takes a different view of the ACA’s legal requirements on this issue. Massachusetts is also the first state to seek a waiver of the federal requirement to include nearly all Food and Drug Administration (FDA)-approved drugs on a state’s formulary. If CMS ultimately approves such a waiver, Massachusetts’ proposal could become a model for other states looking to reduce drug spending.
Notably, the Massachusetts Executive Office of Health and Human Services (EOHHS) has not obtained legislative authorization to implement several of the proposals in the waiver amendment request, including those to implement partial expansion and a closed formulary. It is unclear whether CMS will be willing to approve a proposal that has not been authorized by a state legislature; notably, even if CMS approves the State’s waiver, it cannot be implemented without legislative action.
Key features of the MassHealth waiver amendment request are described in further detail below.
Partial Expansion. Massachusetts is seeking a waiver to limit its Medicaid eligibility level for non-disabled childless adults and parents and caretakers ages 21 to 64 to 100% FPL beginning in January 2019. The State proposes to transition current enrollees with incomes above 100% FPL who meet these criteria to qualified health plans (QHPs) offered on the Connector. This population encompasses approximately 100,000 parents and caretakers and 40,000 expansion adults. Medically frail individuals, pregnant women, women in the breast and cervical cancer treatment program, individuals with HIV, and veterans ineligible for subsidies on the Marketplace are excluded from this proposal and would remain in MassHealth coverage.
Uniquely, Massachusetts has authority under its current 1115 waiver to use Medicaid funding at regular FMAP rates to provide premium and cost-sharing “wrap” subsidies for Marketplace enrollees with incomes up to 300% FPL. Individuals moving from MassHealth to QHP coverage would be eligible for federal subsidies and would have access to at least one QHP with no monthly premium payment.1 In addition, the State intends to align Marketplace co-payment amounts for individuals with incomes between 100% and 133% FPL with those under MassHealth. However, single individuals and families would be subject to maximum annual cost sharing of $1,250 and $2,500, respectively, which are far greater than the maximum of 5% of household income that these groups would be subject to in Medicaid. The State notes that average co-payments for the population transitioning are between $200 and $300 per year.2
Closed Formularies. Massachusetts is proposing a fundamental change to its coverage of prescription drugs, which, if approved, may become a model for other states seeking to reduce drug spending. Under Section 1927 of the Social Security Act, states must include all FDA-approved drugs on their formularies so long as the manufacturers of those drugs provide rebates (this rule is subject to limited exceptions). Massachusetts is proposing a waiver of this requirement to allow the State to adopt a “closed formulary,” which would expand the State’s authority to exclude drugs from its formulary. The State proposes that it would exclude drugs that have inadequate evidence of clinical efficacy. Exclusion from the formulary does not necessarily mean that a drug will not be covered, since an enrollee would still have the option of obtaining such drug through an exceptions process. Massachusetts hopes to leverage this new authority to secure additional supplemental rebates from manufacturers in exchange for coverage, which could ultimately save the State money.
Benefit Package. Massachusetts seeks to transition approximately 230,000 non-disabled parents and caretakers ages 21-64 from the MassHealth Standard benefit package to MassHealth CarePlus, the State’s ABP. With this change, these enrollees would lose access to long-term services and supports (LTSS). Medically frail individuals—generally the enrollees requiring LTSS—would be permitted to remain in MassHealth Standard.
Cost Sharing. The State is seeking to modify MassHealth cost sharing, including to:
- Track cost sharing on an annual instead of a quarterly basis3
- Charge cost sharing beyond 5% of household income for MassHealth enrollees with disabilities who have incomes above 300% FPL and who would not be eligible for Medicaid outside of the demonstration
- Limit ESI and student health insurance premium assistance cost-sharing wrap payments to Medicaid-participating providers, meaning that enrollees covered through premium assistance would be responsible for cost sharing beyond Medicaid limits when they visit non-Medicaid-participating providers
Waiver of the Institutions for Mental Disease (IMD) Exclusion. Under its current 1115 waiver, Massachusetts is authorized to obtain federal matching funds for diversionary behavioral health services and substance use disorder services delivered at IMDs. The State is currently seeking a “waiver of all restrictions on payments to IMDs” for 21- to 64-year-olds, which would grant it flexibility to obtain federal matching funds for additional types of services.
Moving Forward
Unlike states such as Kentucky and Indiana, which seek to impose additional eligibility conditions on Medicaid beneficiaries under the rubric of personal responsibility, Massachusetts’ goal is to further align Medicaid and commercial coverage by expanding the use of the ABP, offering closed formularies and tracking cost sharing on an annual rather than a quarterly basis. Massachusetts offers the same rationale for its request to secure enhanced FMAP for a partial expansion. The changes requested in the Massachusetts waiver will resonate with other state Medicaid agencies, and all stakeholders will be watching to see how far the flexibility promised by the Trump administration will go in practice.
1On September 8, 2017, Massachusetts also submitted to CMS a 1332 waiver application, which proposes creating a premium stabilization fund in lieu of cost-sharing reduction (CSR) payments. Under this proposal, Massachusetts would receive federal pass-through funding reflecting APTC/premium tax credit (PTC) savings due to reduced premiums and waived CSR payments. If this proposal is approved, Massachusetts Connector enrollees would have access to the same level of subsidies as today, but all subsidies would be administered through the premium stabilization fund.
2For an individual with an income of 101% FPL, or $12,180.60 per year, cost sharing of 5% of annual income would equal $609.03.
3Under federal law, states are required to track cost sharing on a quarterly or monthly basis.
Massachusetts Total Healthcare Expenditures: Identifying Cost Drivers
By Kevin McAvey, Senior Manager, Manatt Health
Massachusetts state law (Chapter 224 of the Acts of 2012) requires Massachusetts’ Center for Health Information and Analysis (CHIA) to annually calculate the total amount spent by or on behalf of Massachusetts residents—by private or public payers—for most healthcare services, a per capita (i.e., per state resident) measure known as “Total Healthcare Expenditures” or THCE.1 In September 2016, CHIA reported that THCE increased by 2.8% between 2015 and 2016 to $8,663 per Massachusetts resident, the slowest pace in three years, and below the Commonwealth’s 3.6% benchmark established by the Health Policy Commission (HPC). Sub-population and program spending growth in private commercial, Medicaid/CHIP (MassHealth) and Medicare influenced THCE’s per capita results to varying degrees.2
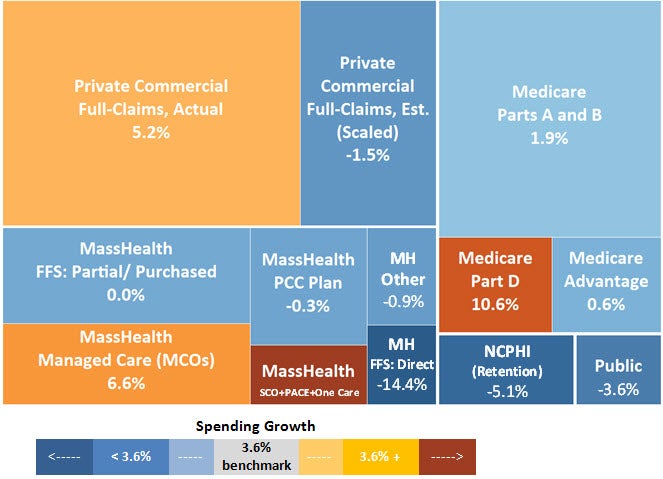
Figure 1 depicts all of THCE’s spending components, scaled to their aggregate spending totals and colored by their per capita growth rates: Components with growth rates above the THCE per capita benchmark are on the yellow/red color scale; components with growth rates below the THCE per capita benchmark are on the blue color scale. Each component’s annual influence on THCE is a combination of the size of its aggregate spending and the magnitude of its per capita spending change. For example, while private commercial,3 MassHealth Managed Care Organization (MCO), Senior Care Options (SCO), Program of All-inclusive Care for the Elderly (PACE), One Care and Medicare Part D pre capita spending growth exceeded Massachusetts’ benchmark, lower spending across the other populations and programs kept overall THCE spending growth below 3.6%.
Figure 1: Total Healthcare Expenditure Components by Size and Per Capita Growth Rate (2015–2016)4
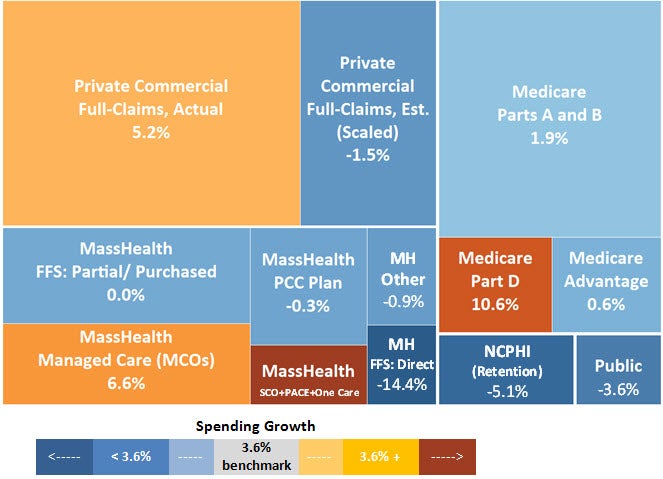
Source: Manatt analysis of data from the Massachusetts Center for Health Information and Analysis’ 2016 Annual Report Databooks.
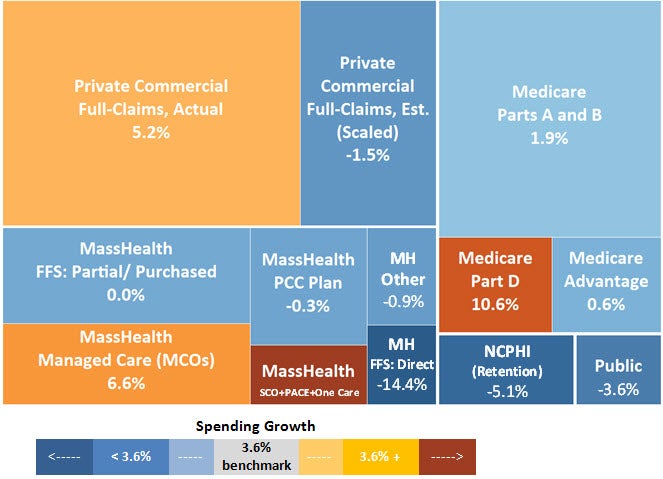
Per capita (i.e., per state resident) spending growth rates alone, however, provide an incomplete picture of Massachusetts’ cost drivers, because they are biased by enrollment shifts and program design changes. In Figure 2, color concentrations show spending changes per member/enrollee for each payer/program grouping between 2015 and 2016 (as opposed to per capita changes reflected in Figure 1). Leveling spending changes to account for enrollment produces several noteworthy findings:
- Though Medicare Part D aggregate spending grew faster than Massachusetts’ THCE benchmark on a per capita basis, when accounting for the influx of new members, Medicare Part D per enrollee spending declined between 2015 and 2016.
- Similarly, though private commercial spending5 pulled Massachusetts’ per capita spending up, once increased private market enrollment is accounted for (including membership growth in Health Connector plans), spending growth on a per member basis was a more modest 3.4%.
- In aggregate and on a per member basis, several large MassHealth spending populations/programs continue to exceed benchmark spending growth levels.
Figure 2: Total Healthcare Expenditure Components by Size and Per Member Per Month Growth Rate (2015–2016)6
Source: Manatt analysis of data from the Massachusetts Center for Health Information and Analysis's 2016 Annual Report Databooks.
Figure 3 depicts how much, on average, is spent per member/enrollee by or on behalf of private commercial,7 Medicare Advantage and Medicaid MCO populations across seven service categories.8 This analysis reflects that, as per member spending growth rates vary between populations and programs, they also vary by service category within populations and programs. For example, average hospital inpatient spending for a Medicare Advantage member was nearly 1.5 times that spent on behalf of the average MassHealth MCO member and private commercial member combined in 2016 ($258 PMPM vs. $178 PMPM combined); however, MassHealth MCO hospital inpatient per member spending growth (8.7%) far outpaced spending growth for either of the other populations.
Source: Manatt analysis of data from the Massachusetts Center for Health Information and Analysis’ 2016 Annual Report Databooks.
For more information on Manatt Health analytics, please contact Kevin McAvey, senior manager, at kmcavey@manatt.com.
1For more information on CHIA’s Total Healthcare Expenditure data, please see CHIA’s recently released Annual Report and related Databooks.
2Population/program spending growth rates shown here are deflated to account for population growth, so as to indicate respective influence on THCE results; values represent the amount of spending by category for all Massachusetts residents, on average.
3Full-claims only (i.e., where carve-out spending did not need to be estimated).
4“MassHealth Other” includes Non-Claims-Based Payments, Non-Capitated Payments, Commonwealth Care Wrap Payments and other MassHealth spending, as reported by MassHealth to CHIA; “Other Public” includes Veterans Affairs, Medical Security Program, Health Safety Net and CommCare spending; “Private Commercial Full-Claims, Est. (Scaled)” includes commercial partial-claim population with actuarial adjustments and compiled spending for non-TME filers with Massachusetts contracts; NCPHI stands for the Net Cost of Private Health Insurance, which includes private commercial, Medicare Advantage and Medicaid MCO/CommCare retention; “MassHealth FFS” includes several programs serving different populations. See CHIA’s Technical Notes for additional information.
5Full-claims only (i.e., where carve-out spending did not need to be estimated).
6Program design and data limitations do not allow for PMPM calculations for “MassHealth Other” and “Other Public.” See CHIA’s Technical Notes for additional information.
7Full-claims only (i.e., where carve-out spending did not need to be estimated).
8CHIA Medicare Advantage aggregate spending and service category totals do not align.
92016 data is preliminary, allowing for only three to four months of claims run-out. See CHIA’s Technical Notes for additional information.
