What Health Plans Should Know About Federal Changes for Dual Eligibles
Editor’s Note: Approximately 12 million people in the United States are dually eligible for both Medicare and Medicaid. Most dual-eligible individuals live below the poverty line and have complex health needs. Because dual-eligible individuals and health plans serving this population must navigate two disparate coverage programs, care is often fragmented and uncoordinated, increasing the risk for poor health outcomes and contributing to disproportionately high costs.
While these problems are years old, the Centers for Medicare & Medicaid Services (CMS) and the states are newly emphasizing a more integrated solution that puts a greater focus on managed care plans addressing the issue: Medicare Advantage (MA) dual-eligible special needs plans (D-SNPs), especially those considered “fully integrated” dual-eligible (FIDE) plans. In 2022, CMS released its Contract Year 2023 Policy and Technical Changes to the Medicare Advantage and Medicare Prescription Drug Benefit Programs final rule. Under this rule, FIDE D-SNPs, or the health plans that offer them, are required to cover both Medicare and Medicaid benefits for the same enrollees and integrate their coverage. Compared with non-FIDE SNPs, FIDE SNPs will earn higher payments as they manage the continuum of covered benefits for their enrollees. But implementing FIDE SNPs requires states and plans to be active participants in developing new coverage models, which presents myriad policy, regulatory and operational challenges.
In a new white paper, summarized below, Manatt Health highlights five key takeaways from the CMS final rule that have important implications for health plans operating in or considering entering the fully integrated duals market. Click here to download the full white paper.
D-SNP Overview
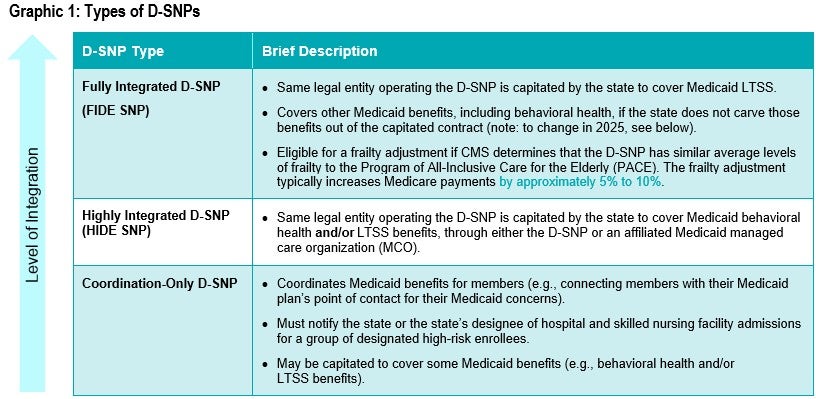
Designed to better coordinate care between Medicare and Medicaid programs, a D-SNP enrolls only dual-eligible individuals. First authorized in 2003, D-SNP enrollment has more than doubled in the past decade, to over four million, and is expected to continue to increase. There are three types of D-SNPs, each providing a different level of Medicare and Medicaid integration (see Graphic 1).
Current D-SNP Market
As of October 2022, over 4.5 million dual-eligible individuals were enrolled in 730 D-SNPs nationwide—half of them in an integrated D-SNP. To promote enrollment in truly integrated products, CMS is not renewing contracts for D-SNP “look-alikes,” MA plans that enroll primarily dual-eligible individuals but are not subject to regulations governing D-SNPs. As a result, an estimated 250,000 dual-eligible individuals will be disenrolled from D-SNP look-alikes and may seek D-SNP coverage.
The current D-SNP landscape, combined with CMS’ defined preference for using FIDE and HIDE SNPs as the integration vehicles for the dual-eligible population, presents significant opportunities for health plans to establish or grow their dual-eligible coverage market presence.
Five Key Takeaways for Health Plans From 2023 CMS Medicare Final Rule
- FIDE SNP enrollment will become more exclusive. Starting in 2025, all FIDE SNPs will only be able to enroll individuals who are receiving Medicaid coverage from the MA’s affiliated Medicaid MCO. Notably, CMS is allowing states to require MA organizations to create separate D-SNP products—one for exclusively aligned enrollment and one or more other product(s) for unaligned enrollment—which would enable MA organizations to keep the FIDE SNP designation for the product with exclusively aligned enrollment. FIDE SNPs will also no longer be able to enroll partial-benefit dual-eligible individuals. Because some FIDE SNPs with unaligned enrollment may need to transition to a HIDE SNP status, such plans run the risk of losing the FIDE SNP frailty adjustment.
- FIDE SNPs will cover a broad array of services. Beginning in 2025, in addition to current benefits, FIDE SNPs will be required to cover Medicaid home health, medical supplies, equipment and appliances, Medicare cost sharing, and behavioral health benefits. FIDE SNPs will no longer be able to operate in states that keep behavioral health carved out of Medicaid managed care or move in the direction of a carve-out in the future.
- States will have the option to require standalone D-SNP contracts. States that have D-SNPs with exclusively aligned enrollment will have the option to require MA organizations to seek CMS approval for standalone, state-specific D-SNP contracts. CMS notes that this contracting structure will help increase transparency, create clearer performance expectations for states and enhance D-SNP oversight efforts. This flexibility may impose a potentially significant administrative burden on health plans to develop separate contracts and may be particularly disruptive for MA organizations with multistate contracts that include D-SNPs. The option also raises some concerns around appropriate quality and performance measures for standalone D-SNP contracts compared to MA contracts that serve fewer dual-eligible individuals. However, the flexibility also presents a potential market opportunity for those health plans that can distinguish themselves by providing high-quality care to D-SNP enrollees.
- With the sunset of the Financial Alignment Initiative (FAI), current Medicare-Medicaid Plans (MMPs) could transition to integrated D-SNPs. CMS will end the current capitated MMP program no later than December 2025 and work with interested states to convert the existing 39 MMPs across nine states to integrated D-SNPs. States interested in converting their MMPs to integrated D-SNPs were required to submit a transition plan to CMS by October 1, 2022. CMS will work with any state opting to forgo the conversion on an appropriate MMP conclusion by December 2023. Plans currently offering an MMP will be forced to wind down or convert their product in line with the state’s MMP transition planning. Prior to CMS’ decision to end the MMP program, participating FAI states may have been less inclined to stand up D-SNPs in order to maximize dual-eligible enrollment in MMPs. With the end of the FAI demonstration, states may lose the opportunity to share in Medicare savings with CMS, a key demonstration authority. As a result, state officials may explore other approaches to achieving savings from investments in integration.
- D-SNPs will be required to solicit enrollee input on the plan. Effective January 1, 2023, MA organizations offering a D-SNP will need to establish one or more enrollee advisory committees in each state to solicit direct input on ways to improve access to covered services, coordination of services and health equity among underserved populations. D-SNPs will have flexibility to determine the frequency, location and participant criteria for enrollee advisory committees. Additionally, state Medicaid agencies have the flexibility to include more prescriptive parameters for enrollee advisory committees in their contracts with D-SNPs. Plans should draw on best practices from existing enrollee engagement efforts and ensure their enrollee advisory committees reflect the demographic diversity of their enrolled populations.
Conclusion
Federal changes to dual-eligible coverage programs are complicated by the broad authority of states to shape their D-SNP markets. Many factors—ranging from Medicaid benefit design to the levels of Medicare expertise and bandwidth among state regulators—can impact state decisions to advance integration through D-SNPs. To set themselves up for success, health plans should leverage opportunities to engage with and educate state officials on the potential of integrated D-SNPs to effectively manage the complex needs of dual-eligible individuals. Plans should also take stock of the characteristics that can help strengthen their position as attractive partners to states, such as a “whole-person” care approach that addresses social drivers of health, commitment to advancing health equity, focus on quality improvement, openness to innovation and active enrollee engagement.
