Oregon’s Glide Path to a Basic Health Program Following the End of Medicaid Continuous Coverage
In December 2022, Oregon became the first state since New York (2015)1 and Minnesota (2016)2 to put forth a plan to seek federal approval for implementation of a basic health program (BHP) under Section 1331 of the Affordable Care Act (ACA) for individuals with income under 200 percent of the federal poverty level (FPL). Oregon is seeking to achieve two primary policy goals in its pursuit of a BHP: (1) preserve the Medicaid coverage gains from the federal COVID-19 public health emergency’s (PHE)3 continuous coverage requirement and (2) expand the role of coordinated care organizations (CCOs)—Oregon’s Medicaid managed care entities—across the state’s various health care coverage programs.
Coverage Gains From the Medicaid Continuous Coverage Requirement in Oregon
In 2021, Oregon’s uninsurance rates dropped to a record low of 4.6 percent, largely due to the continuous coverage provisions instituted during the federal COVID-19 PHE. These coverage gains have been most significant among Black Oregonians—uninsurance dropped from 8 percent to 5 percent from 2019 to 2021—and adults with low incomes (see Figure 1). Coverage gains among individuals in this income category are particularly significant—historically, individuals with incomes from 139 percent to 200 percent of the FPL faced the highest rates of uninsurance in Oregon, reported the highest rates of delayed care due to cost, and had the least access to alternative sources of affordable coverage compared with Oregonians in higher income groups.4
Figure 1. Change in Health Care Insurance Coverage Rates From 2019 to 2021, by Household Income as a Percentage of the FPL
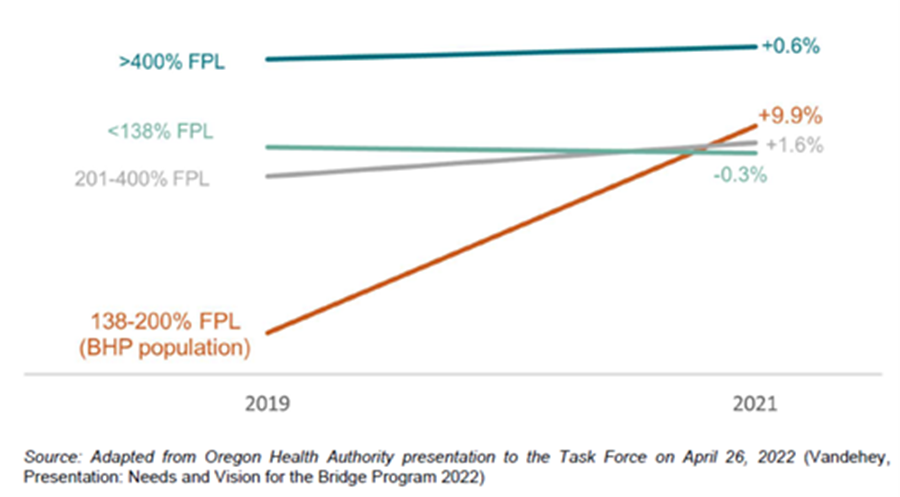
This population is historically susceptible to coverage disruptions. People enrolled in Oregon’s Medicaid program—the Oregon Health Plan (OHP)—are at particular risk for temporarily losing coverage due to administrative reasons, only to qualify again shortly after leaving (known as “churn”). With the federal continuous coverage policy in place, rates of churn have significantly decreased in Oregon, dropping from 34 percent of all individuals enrolling in OHP in 2019 returning after less than a year of leaving to only 8 percent in 2021.5
Beginning April 1, 2023, states again will be required to conduct Medicaid eligibility redeterminations. States will have 12 months to begin conducting redeterminations; once they begin this process, it must be completed within 14 months.6 Millions of Americans face losing Medicaid coverage, including an estimated 300,000 Oregonians.7 For individuals with low incomes, the risk of becoming uninsured is especially high, as they are least likely to have an offer of affordable employer-sponsored coverage and some may find coverage in the health insurance Marketplace unaffordable.
The Glide Path to a Permanent Affordable Coverage Option in Oregon
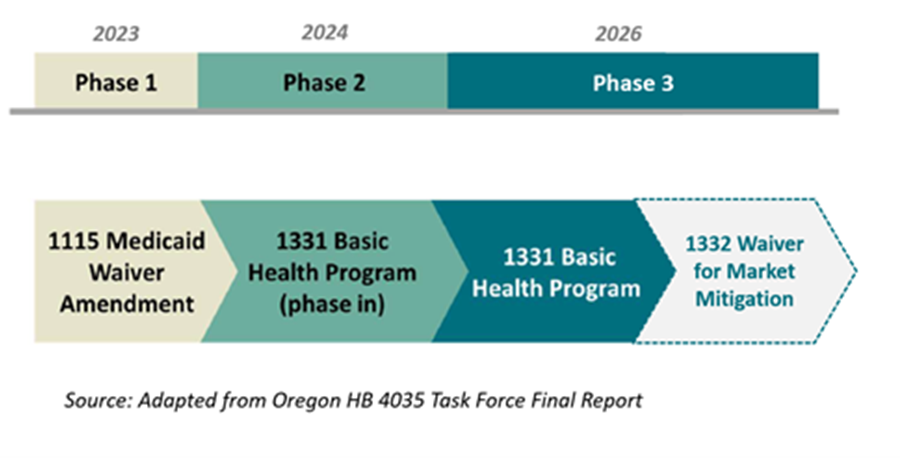
Oregon is taking an incremental approach with its implementation of a permanent affordable coverage option for low-income Oregonians. With an eye toward the end of the federal continuous coverage requirement, Oregon is first seeking a temporary Medicaid section 1115 waiver demonstration amendment (Phase 1) to immediately preserve OHP coverage for individuals with incomes 139 percent to 200 percent of the FPL. The section 1115 waiver would allow individuals enrolled in OHP coverage with a CCO to remain on that same OHP coverage with the same CCO as they had while continuous coverage requirements were in place. This waiver would take effect April 1, 2023, and remain in place until the state implements a BHP.
The state is then seeking to implement a BHP, which would offer benefits that align with the OHP benefits package, have no-to-low premiums and cost-sharing, and be delivered by existing CCOs. Enrollment in the BHP would have two discrete phases.
First, the state would seek to implement a “limited” BHP (Phase 2), meaning only individuals covered under the temporary Medicaid section 1115 waiver (i.e., individuals enrolled in OHP with an income 139 percent to 200 percent of the FPL) would be eligible for BHP coverage. Individuals with incomes from 139 percent to 200 percent of the FPL who are uninsured or enrolled in Marketplace coverage would not be eligible for BHP coverage at this stage. The limited BHP is slated to launch in mid-2024.
Following implementation of the limited BHP, the state would seek to implement a “full” BHP (Phase 3), expanding eligibility to include all individuals in Oregon with incomes 139 percent to 200 percent of the FPL, including individuals who are uninsured or would otherwise be enrolled in Marketplace coverage. The full BHP would be implemented within 24 months of implementation of the limited BHP, meaning no later than January 1, 2026 (see Figure 2 below for summary of Oregon’s proposed glide path).
Mitigating Market Impacts of the BHP
With implementation of a BHP, individuals with incomes between 139 percent and 200 percent of the FPL will no longer be eligible for subsidized coverage in the Marketplace in 2026. This will cause the loss of a pricing strategy known as “silver loading,”8 thus raising premiums for the individuals remaining in the Marketplace. Silver loading occurs when Marketplace plans raise premiums for silver-level Marketplace plans to compensate for cost-sharing reductions that plans are required to provide to certain enrollees who are no longer reimbursed by the federal government. Because silver loading is highest for individuals with incomes below 200 percent of the FPL, removing this population from the Marketplace reduces silver premiums for the remaining Marketplace individuals. Because advance premium tax credits (APTCs) are tied to the cost of the benchmark silver premium, a decreased benchmark plan reduces the buying power of the remaining individuals on the Marketplace.9 As the value of their APTCs goes down, health insurance will become more expensive for many enrollees.
At the same time, by reducing the cost of benchmark plans, Oregon would also be generating federal savings in the form of lowered APTCs. Therefore, the state is seeking a section 1332 waiver to accompany implementation of the full BHP to capture those federal savings and ameliorate the cost impacts of the BHP on the remaining Marketplace enrollees. The state is currently exploring the concept of a gold benchmark (where APTCs would be pegged to the lowest-cost gold plan in a region, rather than the second-lowest-cost silver plan) or a state subsidy (where federal pass-through funds for reduced APTCs would be provided in the form of an additional subsidy for Marketplace enrollees). However, for either of these concepts, Oregon may require a state-based Marketplace to implement it, which could delay implementation of Phase 3.
Figure 2. Oregon’s Proposed Glide Path to a Full BHP
Expanding the Role of CCOs in Oregon
Central to Oregon’s plan to implement a BHP are the state’s CCOs. CCOs are at the forefront of many of the state’s broader goals for health equity, health access and the adoption of value-based payment (VBP) models. For example, Oregon’s CCO program includes innovations such as services centered on the social determinants of health, culturally and linguistically appropriate services and supports, and access to traditional health workers.10 In addition, the Medicaid CCO market has a higher share of pay-for-performance VBP models compared with other markets in the state.11 Though Oregon had previously pursued a broader goal of extending CCOs to serve the entire Marketplace as part of the state’s public option plan, the state has now narrowed its goal to focus its CCO expansion on the BHP population instead, which is far less disruptive to the Marketplace and also highly compatible with the goal of smoothing the coverage continuum for a low-income population facing the possibility of becoming uninsured amid Medicaid redeterminations.12
Conclusion
Oregon is the first state to pursue a BHP as part of its strategy for maintaining continuous coverage for low-income adults at risk of losing coverage in the unwinding of the continuous coverage requirement. Other states can leverage Oregon’s proposal to see whether similar approaches may be viable options to reduce churn and avoid uninsurance during this uncertain time for Medicaid enrollees.
1 Essential Plan, New York Basic Health Program Blueprint Submission. April 2015. Available here.
2 MinnesotaCare, Minnesota Basic Health Program Blueprint Submission. February 2016. Available here.
3 Polaris, J. Federal Declarations and Flexibilities Supporting Medicaid and CHIP COVID-19 Response Efforts Effective and End Dates. Manatt Health for State Health & Value Strategies. October 2022. Available here.
4 Vandehey, J. Direction & Vision for Bridge Program. May 2022. Available here.
5 Vandehey, J., Hittle, D., and Flowers, C. Oregon Health Plan Post-Public Health Emergency Eligibility Redeterminations Planning. Oregon Health Authority. Presented to the Oregon House Health Care Committee. February 2022. Available here.
6 Pub. L. 117-328, Consolidated Appropriations Act of 2023.
7 Vandehey, J. Unwinding Federal Public Health Emergency and OHP Continuous Coverage Policies. Presented to the Bridge Program Task Force. April 2022. Oregon Health Authority. Available here.
8 Fiedler, M. The Case for Replacing “Silver Loading.” May 2021. Available here.
9 The benchmark is the second-lowest-cost silver premium available to an individual.
10 Oregon Department of Human Services. Who Is a Traditional Health Worker? Available here.
11 Oregon Health & Science University. Prepared for the Oregon Health Authority. Oregon’s Value-Based Payment Roadmap for Coordinated Care Organizations. December 2022. Available here.
12 Ario, J., Karl, A., and Zhan, A. Oregon Health Authority Public Option Implementation Report. January 2022. Available here.
