COVID-19-Related Flexibilities: Moving Toward More Person-Centered Medicare and Medicaid Programs
Editor’s Note: Over the course of the COVID-19 public health emergency (PHE), a series of Medicare and Medicaid regulatory flexibilities were implemented to help ensure access to care for older adults and people with chronic conditions or disabilities by minimizing administrative, clinical and financial barriers to using services. As the temporary flexibilities will end upon or shortly after the end of the PHE, policymakers must decide whether and which temporary flexibilities should be made permanent because they advance person- and community-centered care and promote health equity beyond the PHE.
In a new issue brief and companion playbook prepared by Manatt Health and Health Management Associates (HMA) for The SCAN Foundation, we provide a person-centered assessment framework to aid policymakers in making these complex decisions. The issue brief, summarized below, examines the benefits and risks of COVID-19 flexibilities, describes the person-centered assessment framework, and offers recommendations for flexibilities that should be considered for permanence. The companion playbook is an actionable guide for using the person-centered assessment framework and describes potential authorities for making flexibilities permanent. Click here to download free copies of the full issue brief and playbook.
The temporary regulatory flexibilities implemented during the PHE expanded program eligibility and enrollment, enhanced remote service delivery options, authorized care delivery in alternative care sites, and much more. Although the federal PHE has been extended to April 15, 2022, these regulatory flexibilities are temporary and will inevitably end when policymakers terminate the PHE.1
As policymakers prepare for the unwinding of these temporary policies, they have the unique opportunity to assess the policies’ impact on advancing person- and community-centered care and consider flexibilities for permanence through this lens. In this context, person-centered care means health care that is guided by an individual’s personal values and preferences and is designed to help people achieve what matters most to them. Community-centered care is an approach to care that involves expanding care outside the walls of clinical providers and into communities in a way that helps individuals directly engage in addressing the factors contributing to their health status. Yet policymakers and other stakeholders have only started to understand the impact of these flexibilities on health care consumers and the providers and systems that provide their care.
Uneven data collection and reporting across the Medicare and Medicaid flexibilities and populations during the pandemic inhibited a comprehensive analysis of the impact of the flexibilities on consumer access, service utilization and outcomes, and the provider and direct care workforce. The limited quantitative data that do exist indicate that telehealth flexibilities facilitate access to timely care in individuals’ homes or communities. Qualitative data are more abundant and support the use of telehealth and provider workforce flexibilities to improve access to care but suggest that certain flexibilities may widen health disparities or harm patient care if not implemented with modifications designed to ameliorate these risks.
At the outset of the pandemic, regulatory flexibilities were implemented quickly to minimize disruptions in access to care. In many cases, the regulatory changes aligned Medicare and Medicaid program policies that were previously misaligned; for example, Medicare temporarily allows patients to use telehealth in their homes, similar to pre-COVID-19 policies in many states. Without further federal or state action to adopt temporary flexibilities as permanent policy, a return to pre-pandemic rules will result in a return to the complex regulatory web that consumers and providers had to navigate prior to 2020.
A Person-Centered Assessment Framework to Facilitate Decisions
As policymakers consider which temporary regulatory flexibilities might improve the Medicare and Medicaid programs if continued as permanent policies, they are now faced with complex decisions weighing the impact on consumers and providers, the opportunities for programmatic alignment, the ability of modifications to address risks, and the possibility of additional evaluation before making a final choice.
Manatt Health and HMA conceptualized a person-centered assessment framework to facilitate these decisions. The framework assesses the potential for the regulatory flexibilities to:
- Advance person- and community-centered care
- Facilitate care in the least intensive or least restrictive setting
- Better align Medicare and Medicaid program rules
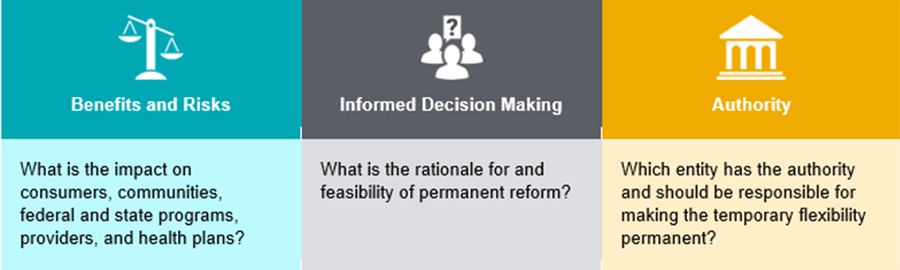
The person-centered assessment framework was tested and refined with a diverse group of stakeholders, including consumers and consumer advocates, experts in diversity, equity and inclusion (DEI), health plans and providers, state officials, and former federal officials, to ensure it would be an actionable tool for federal and state policymakers. The person-centered assessment framework is organized into the following three sections, each with probing questions for policymakers to consider as they deploy the tool:
Using the person-centered assessment framework and informed by stakeholders, Manatt Health and HMA identified several priority COVID-19 temporary regulatory flexibilities to consider for permanence, additional modification or further evaluation. We intend these recommendations to be viewed through the lens of advancing person- and community-centered care for older adults and people with chronic conditions or disabilities. To that end, we identify flexibilities that should be considered for permanence if person- and community-centered care is the primary goal, recognizing that policymakers face numerous additional trade-offs when making policy decisions.
These flexibilities fall under four major categories and were selected based on their ability to promote person- and community-centered care in the least intensive or least restrictive setting and better align Medicare and Medicaid program rules and policies (Table 2).
Table 2. Categories of COVID-19-Related Temporary Regulatory Flexibilities That Enhance Person-Centered Care in Medicare and Medicaid
| Category | Description | |
| Expand Telehealth Benefits | Targeted and equitable expansion of remote care delivery opportunities, particularly telehealth, for all beneficiaries | |
| Modify Provider Scope of Practice and Related Requirements | Modifications to provider licensure, scope of practice, qualifications and payment rates to strengthen and expand the workforce (clinical providers, direct care workers and paid family caregivers) | |
| Modify Medicare Advantage (MA) Requirements | Modifications to MA requirements related to telehealth, risk adjustment and midyear benefit enhancements to support person-centered care | |
| Other Temporary Flexibilities | Adjustments to other Medicare and Medicaid program requirements such as three-day prior hospitalization requirement for skilled nursing facility (SNF) stays, self-directed home- and community-based services (HCBS), and long-term services and supports (LTSS) financial eligibility rules | |
The person-centered assessment framework and priority list of flexibilities for permanence or further evaluation are foundational tools for policymakers hoping to advance person-centered and community-centered care in Medicare and Medicaid.
Moving Beyond the Pandemic
The COVID-19 pandemic has had a devastating and lasting impact on American society. It also has presented a unique opportunity for federal and state policymakers to evaluate Medicare and Medicaid policies designed to ensure access to care for older adults and people with chronic conditions or disabilities. The temporary regulatory flexibilities granted during the pandemic enabled people to safely obtain person-centered care in their homes and communities, expanded access to services, and bolstered an essential yet struggling provider and direct care workforce. While there is limited data available to date, existing evidence indicates that flexibilities positively affected consumers, providers and payers. More evaluation is needed to understand the impact of these flexibilities and to assess the impact of flexibilities that have yet to be measured, particularly with respect to how flexibilities advance person- and community-centered care and advance health equity.
1 The Centers for Medicare and Medicaid Services (CMS) recently confirmed the Biden Administration’s commitment to provide states with 60 days’ notice prior to ending the PHE. Because such notice has not been given within the 60-day period prior to April 15, 2022, the PHE likely will be extended through July 15, 2022.
