Manatt Telehealth Policy Tracker: Tracking Ongoing Federal and State Telehealth Policy Changes
Purpose: The purpose of this tracker is to summarize major federal and state actions related to telehealth and digital health policy and to highlight emerging statutory and regulatory changes shaping virtual care delivery. This update captures activity from August 1, 2025-November 20, 2025.
At the federal level, Congress ended the 43-day government shutdown on November 12, 2025, by enacting H.R. 5371, which temporarily reinstates several Medicare telehealth flexibilities that had lapsed on October 1 following the expiration of H.B. 1968 through January 30, 2026. Across the states, 11 newly enacted bills refine telehealth frameworks—expanding licensure and practice flexibilities in some jurisdictions while imposing modality- or service-specific limits in others.
New Federal Developments
Item | Activity |
|---|---|
, the “Continuing Appropriations, Agriculture, Legislative Branch, Military Construction and Veterans Affairs, and Extensions Act, 2026” | Impact of the Federal Government Shutdown on Medicare Telehealth Coverage:
|
New State-Level Developments
State | Activity |
|---|---|
Delaware |
|
Illinois |
|
Missouri |
|
New Jersey |
|
North Carolina |
|
Oregon |
|
Texas |
|
Wisconsin |
|
Telehealth Payment Parity: State-by-State Tracker
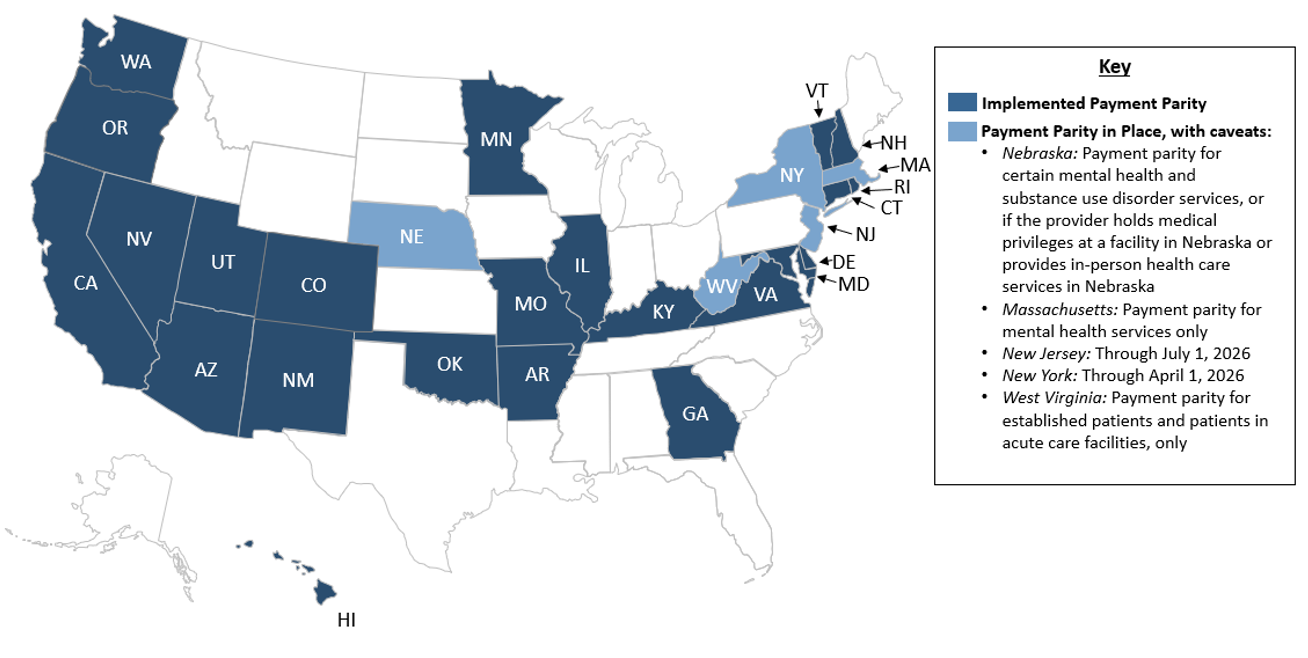
“Payment parity” requires payors to reimburse for telehealth at the same rate as the equivalent in-person service. Prior to the COVID-19 pandemic, roughly ten states had implemented payment parity for telehealth (i.e., video visits). Many states implemented temporary payment parity following the onset of the pandemic; since then, several states passed laws implementing payment parity either permanently or with caveats (e.g., on a temporary basis, limited to specific specialties).
Payment parity policies are typically codified in state laws, statutes, or regulations that outline coverage and reimbursement requirements for payors. The Manatt Telehealth Policy Tracking team has analyzed the relevant payment parity policies in each state to develop the map and table below; these are updated on a quarterly basis. The map below indicates states that have implemented payment parity permanently or with caveats; the table includes supporting language from each state’s relevant law, statute, or regulation.
Map of States with Laws Requiring Payment Parity (As of November 20, 2025)
As of November 2025, 23 states have implemented payment parity, five states have payment parity in place with caveats, and 22 states have no payment parity requirement.
State-by-State Payment Parity Requirements Table
The table below includes state law, statute, or regulatory telehealth reimbursement requirements relevant to insurers (commercial, Medicaid, others), and indicates whether each state requires payors to reimburse providers for the delivery of telehealth services at parity with in-person care.
State | Payment Parity: Does state law, statute, or regulatory requirements require that insurers (commercial, Medicaid, others) reimburse for services delivered via video visit at the same rate as those delivered in-person? |
|---|---|
Alabama | No. No relevant policy or statue reference found. |
Alaska | No, mental health coverage parity only. “A health care insurer that offers, issues for delivery, or renews in the state a health care insurance plan in the group or individual market [THAT PROVIDES MENTAL HEALTH BENEFITS] shall provide coverage for [MENTAL HEALTH] benefits provide through telehealth by a health care provider licensed in this state and may not require that prior in-person contact occur between a health care provider and a payment before payment is made for covered services.” – (Accessed May 2021) |
Arizona | Yes. “2. Except as otherwise provided in this paragraph, a corporation shall reimburse health care providers at the same level of payment for equivalent services as identified by the healthcare common procedure coding system, whether provided through telehealth using an audio-visual format or in-person care. A corporation shall reimburse health care providers at the same level of payment for equivalent in-person behavioral health and substance use disorder services as identified by the healthcare common procedure coding system if provided through telehealth using an audio-only format. This paragraph does not apply to a telehealth encounter provided through a telehealth platform that is sponsored or provided by the corporation.” – (Accessed May 2021) |
Arkansas | Yes. “(2) (A) ‘Health benefit plan’ means: (i) An individual, blanket, or group plan, policy, or contract for healthcare services issued or delivered by an insurer, health maintenance organization, hospital medical service corporation, or self-insured governmental or church plan in this state; and (ii) Any health benefit program receiving state or federal appropriations from the State of Arkansas, including the Arkansas Medicaid Program, the Health Care Independence Program, commonly referred to as the "Private Option", and the Arkansas Works Program, or any successor program. (1) A health benefit plan shall provide coverage and reimbursement for healthcare services provided through telemedicine on the same basis as the health benefit plan provides coverage and reimbursement for health services provided in person, unless this subchapter specifically provides otherwise. (2) A health benefit plan is not required to reimburse for a healthcare service provided through telemedicine that is not comparable to the same service provided in person.” – and (Accessed May 2021) |
California | Yes, except for Medi-Cal managed care plans. “(a) (1) A contract issued, amended, or renewed on or after January 1, 2021, between a health care service plan and a health care provider for the provision of health care services to an enrollee or subscriber shall specify that the health care service plan shall reimburse the treating or consulting health care provider for the diagnosis, consultation, or treatment of an enrollee or subscriber appropriately delivered through telehealth services on the same basis and to the same extent that the health care service plan is responsible for reimbursement for the same service through in-person diagnosis, consultation, or treatment. (f) This section shall not apply to Medi-Cal managed care plans that contract with the State Department of Health Care Services pursuant to Chapter 7 (commencing with Section 14000) of, Chapter 8 (commencing with Section 14200) of, or Chapter 8.75 (commencing with Section 14591) of, Part 3 of Division 9 of the Welfare and Institutions Code.” – (Accessed May 2021) |
Colorado | Yes. “(b) (I) Subject to all terms and conditions of the health benefit plan, a carrier shall reimburse the treating participating provider or the consulting participating provider for the diagnosis, consultation, or treatment of the covered person delivered through telehealth on the same basis that the carrier is responsible for reimbursing that provider for the provision of the same service through in-person consultation or contact by that provider.” – (Accessed May 2021) |
Connecticut | Yes, for Medicaid services only. “(b) Notwithstanding the provisions of section 17b-245c, 17b-245e or 204 19a-906 of the general statutes, as amended by this act, or any other section of the general statutes, regulation, rule, policy or procedure governing the Connecticut medical assistance program, the Commissioner of Social Services shall, to the extent permissible under federal law, provide coverage under the Connecticut medical assistance program for audio-only telehealth services when (1) clinically appropriate, as determined by the commissioner, (2) it is not possible to provide comparable covered audiovisual telehealth services, and (3) provided to individuals who are unable to use or access comparable, covered audiovisual telehealth services. (c) To the extent permissible under federal law, the commissioner shall provide Medicaid reimbursement for services provided by means of telehealth to the same extent as if the service was provided in person.” – (Accessed June 2021) |
Delaware | Yes. “(e) An insurer, health service corporation, or health maintenance organization shall reimburse the treating provider or the consulting provider for the diagnosis, consultation, or treatment of the insured delivered through telemedicine services on the same basis and at least at the rate that the insurer, health service corporation, or health maintenance organization is responsible for coverage for the provision of the same service through in-person consultation or contact. Payment for telemedicine interactions shall include reasonable compensation to the originating or distant site for the transmission cost incurred during the delivery of health-care services.” – (Accessed May 2021) |
District of Columbia | No. “(b) A health insurer shall reimburse the provider for the diagnosis, consultation, or treatment of the insured when the service is delivered through telehealth.” – (Accessed May 2021) |
Florida | No. “(45) A contract between a health maintenance organization issuing major medical individual or group coverage and a telehealth provider, as defined in s. 456.47, must be voluntary between the health maintenance organization and the provider and must establish mutually acceptable payment rates or payment methodologies for services provided through telehealth. Any contract provision that distinguishes between payment rates or payment methodologies for services provided through telehealth and the same services provided without the use of telehealth must be initialed by the telehealth provider.” – (Accessed May 2021) |
Georgia | Yes. “(3) ‘Insurer’ means an accident and sickness insurer, fraternal benefit society, hospital service corporation, medical service corporation, health care corporation, health maintenance organization, provider sponsored health care corporation, managed care entity, or any similar entity authorized to issue contracts under this title or to provide health benefit policies. (f) An insurer shall reimburse the treating provider or the consulting provider for the diagnosis, consultation, or treatment of the insured delivered through telemedicine services on the same basis and at least at the rate that the insurer is responsible for coverage for the provision of the same service through in-person consultation or contact; provided, however, that nothing in this subsection shall require a health care provider or telemedicine company to accept more reimbursement than they are willing to charge. Payment for telemedicine interactions shall include reasonable compensation to the originating or distant site for the transmission cost incurred during the delivery of health care services.” – (Accessed May 2021) |
Hawaii | Yes. “(c) Reimbursement for services provided through telehealth via an interactive telecommunications system shall be equivalent to reimbursement for the same services provided via in-person contact between a health care provider and a patient; provided that reimbursement for two-way, real-time audio-only communication technology for purposes of diagnosis, evaluation, or treatment of a mental health disorder to a patient in the patient’s home shall be equivalent to eighty per cent of the reimbursement for the same services provided via in-person contact between a health care provider and a patient. To be reimbursed for telehealth via an interactive telecommunications system using two-way, real-time audio-only communication technology in accordance with this subsection, the health care provider shall first conduct an in-person visit or a telehealth visit that is not audio only, within six months prior to the initial audio-only visit, or within twelve months prior to any subsequent audio-only visit. The telehealth visit required prior to the initial or subsequent audio-only visit in this subsection shall not be provided using audio-only communication. Nothing in this section shall require a health care provider to be physically present with the patient at an originating site unless a health care provider at the distant site deems it necessary.” “This Act shall take effect upon its approval; provided that on December 31, 2025, this Act shall be repealed and sections 346–59.1, 431:10A–116.3, 432:1–601.5, 432D–23.5, and 453–1.3, Hawaii Revised Statutes, shall be reenacted in the form in which they read on the day prior to the effective date of this Act.” – (October 2024) “(c) Reimbursement for services provided through telehealth shall be equivalent to reimbursement for the same services provided via face-to-face contact between a health care provider and a patient. Nothing in this section shall require a health care provider to be physically present with the patient at an originating site unless a health care provider at the distant site deems it necessary.” – (Accessed May 2021) (Note: HI Revised Statutes, accessed October 2023, does not appear to yet incorporate the changes made by HI Act 107 (see above)) |
Idaho | No. No relevant policy or statue reference found. |
Illinois | Yes. “(d) For purposes of reimbursement, an individual or group policy of accident or health insurance that is amended, delivered, issued, or renewed on or after the effective date of this amendatory Act of the 102nd General Assembly shall reimburse an in-network health care professional or facility, including a health care professional or facility in a tiered network, for telehealth services provided through an interactive telecommunications system on the same basis, in the same manner, and at the same reimbursement rate that would apply to the services if the services had been delivered via an in-person encounter by an in-network or tiered network health care professional or facility. This subsection applies only to those services provided by telehealth that may otherwise be billed as an in-person service. This subsection is inoperative on and after January 1, 2028, except that this subsection is operative after that date with respect to mental health and substance use disorder telehealth services.” – (Accessed August 2021) |
Indiana | No, coverage parity only. “Sec. 6. (a) A policy must provide coverage for telemedicine services in accordance with the same clinical criteria as the policy provides coverage for the same health care services delivered in person.” – (Accessed May 2021) |
Iowa | No, not explicitly. “2. Notwithstanding the uniformity of treatment requirements of section 514C.6, a policy, contract, or plan providing for third-party payment or prepayment of health or medical expenses shall not discriminate between coverage benefits for health care services that are provided in person and the same health care services that are delivered through telehealth.” – (Accessed May 2021) |
Kansas | No, not explicitly. “(d) Payment or reimbursement of covered healthcare services delivered through telemedicine may be established by an insurance company, nonprofit health service corporation, nonprofit medical and hospital service corporation or health maintenance organization in the same manner as payment or reimbursement for covered services that are delivered via in-person contact are [is] established.” – (Accessed May 2021) |
Kentucky | Yes. “(1)(a) A health benefit plan shall reimburse for covered services provided to an insured person through telehealth as defined in KRS 304.17A-005. Telehealth coverage and reimbursement shall be equivalent to the coverage for the same service provided in person unless the telehealth provider and the health benefit plan contractually agree to a lower reimbursement rate for telehealth services.” – (Accessed May 2021) |
Louisiana | No. “Notwithstanding any provision of any policy or contract of insurance or health benefits issued, whenever such policy provides for payment, benefit, or reimbursement for any health care service, including but not limited to diagnostic testing, treatment, referral, or consultation, and such health care service is performed via transmitted electronic imaging or telemedicine, such a payment, benefit, or reimbursement under such policy or contract shall not be denied to a licensed physician conducting or participating in the transmission at the originating health care facility or terminus who is physically present with the individual who is the subject of such electronic imaging transmission and is contemporaneously communicating and interacting with a licensed physician at the receiving terminus of the transmission. The payment, benefit, or reimbursement to such a licensed physician at the originating facility or terminus shall not be less than seventy-five percent of the reasonable and customary amount of payment, benefit, or reimbursement which that licensed physician receives for an intermediate office visit.” – (Accessed May 2021) |
Maine | No. “A carrier offering a health plan in this State may not deny coverage on the basis that the health care service is provided through telehealth if the health care service would be covered if it were provided through in-person consultation between an enrollee and a provider. Coverage for health care services provided through telehealth must be determined in a manner consistent with coverage for health care services provided through in-person consultation… . A carrier may offer a health plan containing a provision for a deductible, copayment or coinsurance requirement for a health care service provided through telehealth as long as the deductible, copayment or coinsurance does not exceed the deductible, copayment or coinsurance applicable to a comparable service provided through in-person consultation.” – (Accessed May 2021) |
Maryland | Yes. “When appropriately provided via telehealth, the Program shall provide reimbursement in accordance with paragraph (1)(i) of this subsection on the same basis and the same rate as if the health care service were delivered by the health care provider in person” – (Accessed May 2025) |
Massachusetts | Yes, but only for mental health services. “Insurance companies organized under this chapter shall ensure that the rate of payment for in-network providers of behavioral health services delivered via interactive audio video technology and audio-only telephone shall be no less than the rate of payment for the same behavioral health service delivered via in-person methods; provided, that this subsection shall apply to providers of behavioral health services covered as required under subclause (i) of clause (4) of the second sentence of subsection (a) of section 6 of chapter 1760.” “Medical service corporations shall ensure that the rate of payment for in-network providers of behavioral health services delivered via interactive audio-video technology and audio-only telephone shall be no less than the rate of payment for the same behavioral health service delivered via in-person methods.” – (Accessed May 2021) The same language is repeated for hospital service corporations and health maintenance organizations for behavioral health services delivered via telehealth. |
Michigan | No, not explicitly. “An insurer that delivers, issues for delivery, or renews in this state a health insurance policy shall not require face-to-face contact between a health care professional and a patient for services appropriately provided through telemedicine, as determined by the insurer. Telemedicine services must be provided by a health care professional who is licensed, registered, or otherwise authorized to engage in his or her health care profession in the state where the patient is located. Telemedicine services are subject to all terms and conditions of the health insurance policy agreed upon between the policy holder and the insurer, including, but not limited to, required copayments, coinsurances, deductibles, and approved amounts. If a service is provided through telemedicine under this section, the insurer shall provide at least the same coverage for that service as if the service involved face-to-face contact between the health care professional and the patient.” (Accessed June 2024) After December 31, 2017, “insurer” includes a nonprofit dental care corporation operating under 1963 PA 125, MCL 550.351 to 550.373. – (Accessed June 2024) |
Minnesota | Yes. “‘Health carrier’ means an insurance company licensed under chapter 60A to offer, sell, or issue a policy of accident and sickness insurance as defined in section ; a nonprofit health service plan corporation operating under chapter 62C; a health maintenance organization operating under chapter 62D; a fraternal benefit society operating under chapter 64B; or a joint self-insurance employee health plan operating under chapter 62H.” – (Accessed May 2021) “(a) A health carrier must reimburse the health care provider for services delivered through telehealth on the same basis and at the same rate as the health carrier would apply to those services if the services had been delivered by the health care provider through in-person contact.” – (Accessed May 2021) |
Mississippi | No, coverage parity only. “All health insurance and employee benefit plans in this state must provide coverage for telemedicine services to the same extent that the services would be covered if they were provided through in-person consultation.” – . (Accessed March 2025) |
Missouri | Yes. “(22) ‘Health carrier’, an entity subject to the insurance laws and regulations of this state that contracts or offers to contract to provide, deliver, arrange for, pay for or reimburse any of the costs of health care services, including a sickness and accident insurance company, a health maintenance organization, a nonprofit hospital and health service corporation, or any other entity providing a plan of health insurance, health benefits or health services; except that such plan shall not include any coverage pursuant to a liability insurance policy, workers’ compensation insurance policy, or medical payments insurance issued as a supplement to a liability policy” – (Accessed May 2021) “Each health carrier or health benefit plan that offers or issues health benefit plans which are delivered, issued for delivery, continued, or renewed in this state on or after January 1, 2014, shall not deny coverage for a health care service on the basis that the health care service is provided through telehealth if the same service would be covered if provided through face-to-face diagnosis, consultation, or treatment.” “A health carrier shall not be required to reimburse a telehealth provider or a consulting provider for site origination fees or costs for the provision of telehealth services; however, subject to correct coding, a health carrier shall reimburse a health care provider for the diagnosis, consultation, or treatment of an insured or enrollee when the health care service is delivered through telehealth on the same basis that the health carrier covers the service when it is delivered in person.” – (Accessed May 2021) |
Montana | No, coverage parity only. “Each group or individual policy, certificate of disability insurance, subscriber contract, membership contract, or health care services agreement that provides coverage for health care services must provide coverage for health care services provided by a health care provider or health care facility by means of telehealth if the services are otherwise covered by the policy, certificate, contract, or agreement.” – (Accessed May 2021) |
Nebraska | Yes, but only for certain mental health and substance use disorder services or if the provider holds medical privileges at a facility in Nebraska or provides in-person health care services in Nebraska. “Any health insurance plan delivered, issued, or renewed in this state if coverage is provided for treatment of mental health conditions other than alcohol or substance abuse, shall provide a reimbursement rate for accessing treatment for a mental health condition using telehealth services that is the same as the rate for a comparable treatment provided or supervised in person.” – (Accessed March 2022) “3)(a) Any insurer offering any policy, certificate, contract, or plan described in subsection (2) of this section for which coverage of benefits begins on or after January 1, 2021, shall not exclude from coverage telehealth services provided by a dermatologist solely because the service is delivered asynchronously. (b) An insurer shall reimburse a health care provider for asynchronous review by a dermatologist delivered through telehealth at a rate negotiated between the provider and the insurer.” – (Accessed May 2021) “Except as otherwise provided in section 44-793, the reimbursement rate for any telehealth service shall, at a minimum, be the same as a comparable in-person health care service if the licensed provider providing the telehealth service also provides in-person health care services at a physical location in Nebraska or is employed by or holds medical staff privileges at a licensed facility in Nebraska and such facility provides in-person health care services in Nebraska.” – (Accessed September 2023) |
Nevada | Yes. “A policy of health insurance subject to the provisions of this chapter that is delivered, issued for delivery or renewed on or after October 1, 2021, has the legal effect of including the coverage required by this section, and any provision of the policy or the renewal which is in conflict with this section is void. A policy of health insurance must include coverage for services provided to an insured through telehealth to the same extent and, except for services provided through audio-only interaction, in the same amount as though provided in person or by other means.” – (Accessed August 2021) |
New Hampshire | Yes. “An insurer offering a health plan in this state shall provide coverage and reimbursement for health care services provided through telemedicine on the same basis as the insurer provides coverage and reimbursement for health care services provided in person.” – (Accessed May 2021) |
New Jersey | Yes, through July 1, 2026. “For the period beginning on the effective date of P.L.2021, c.310 and ending on July 1, 2026, a health benefits plan in this State shall provide coverage and payment for health care services delivered to a covered person through telemedicine or telehealth at a provider reimbursement rate that equals the provider reimbursement rate that is applicable, when the services are delivered through in-person contact and consultation in New Jersey, provided the services are otherwise covered by the health benefits plan when delivered through in-person contact and consultation in New Jersey. The requirements of this subsection shall not apply to: (1) a health care service provided by a telemedicine or telehealth organization that does not provide the health care service on an in-person basis in New Jersey; or (2) a physical health care service that was provided through real-time, two-way audio without a video component, whether or not utilized in combination with asynchronous store-and-forward technology, including through audio-only telephone conversation. The reimbursement rate for a physical health care service that is subject to this paragraph shall be determined under the contract with the provider; provided that the reimbursement rate for a physical health care service when provided through audio-only telephone conversation shall be at least 50 percent of the reimbursement rate for the service when provided in person. (3) The provisions of paragraph (2) of this subsection shall not apply to a behavioral health service that was provided through real-time, two-way audio without a video component, whether or not utilized in combination with asynchronous store-and-forward technology, including audio-only telephone conversation. A behavioral health care service described in this paragraph shall be reimbursed at a rate that equals the provider reimbursement rate for the service when provided in person.” – (Accessed January 2025) |
New Mexico | Yes. “An insurer shall reimburse for health care services delivered via telemedicine on the same basis and at least the same rate that the insurer reimburses for comparable services delivered via in-person consultation or contact.” – (Accessed May 2021) |
New York | Yes, through April 1, 2026. “(2) An insurer that provides comprehensive coverage for hospital, medical or surgical care shall reimburse covered services delivered by means of telehealth on the same basis, at the same rate, and to the same extent that such services are reimbursed when delivered in person; provided that reimbursement of covered services delivered via telehealth shall not require reimbursement of costs not actually incurred in the provision of the telehealth services, including charges related to the use of a clinic or other facility when neither the originating site nor distant site occur within the clinic or other facility.” – (Accessed May 2024) “7. This act shall take effect immediately and shall be deemed to have been in full force and effect on and after April 1, 2022; provided, however, this act shall expire and be deemed repealed on and after April 1, 2026.” – (Accessed May 2024) |
North Carolina | No. No relevant policy or statue reference found. |
North Dakota | No, not explicitly. “Payment or reimbursement of expenses for covered health services delivered by means of telehealth under this section may be established through negotiations conducted by the insurer with the health services providers in the same manner as the insurer with the health services providers in the same manner as the insurer establishes payment or reimbursement of expenses for covered health services that are delivered by in-person means.” – (Accessed May 2021) |
Ohio | No, coverage parity only. “A health benefit plan shall provide coverage for telemedicine services on the same basis and to the same extent that the plan provides coverage for in-person health care services. Plans cannot exclude coverage for a service solely because it is provided as a telemedicine service.” – (Accessed May 2021) “(D) This section shall not be construed as doing any of the following: […] (3) Requiring a health plan issuer to reimburse a telemedicine provider for telemedicine services at the same rate as in-person services. (E) This section applies to all health benefit plans issued, offered, or renewed on or after January 1, 2021.” – (Accessed May 2021) |
Oklahoma | Yes. “‘Insurer’ means any entity providing an accident and health insurance policy in this state including, but not limited to, a licensed insurance company, a not-for-profit hospital service and medical indemnity corporation, a fraternal benefit society, a multiple employer welfare arrangement or any other entity subject to regulation by the Insurance Commissioner; […] An insurer shall reimburse the treating health care professional or the consulting health care professional for the diagnosis, consultation or treatment of the patient delivered through telemedicine services on the same basis and at least at the rate of reimbursement that the insurer is responsible for coverage for the provision of the same, or substantially similar, services through in-person consultation or contact. This act shall become effective January 1, 2022.” – (Accessed May 2021) |
Oregon | Yes. “(2) To encourage the efficient use of resources and to promote cost-effective procedures in accordance with ORS 413.011 (1)(L), the Oregon Health Authority shall reimburse the cost of health services delivered using telemedicine, including but not limited to: (a) Health services transmitted via landlines, wireless communications, the Internet and telephone networks; (b) Synchronous or asynchronous transmissions using audio only, video only, audio and video and transmission of data from remote monitoring devices; and (c) Communications between providers or between one or more providers and one or more patients, family members, caregivers or guardians. (3)(a) The authority shall pay the same reimbursement for a health service regardless of whether the service is provided in person or using any permissible telemedicine application or technology. […] (8)(a) A health benefit plan and dental-only plan must pay the same reimbursement for a health service regardless of whether the service is provided in person or using any permissible telemedicine application or technology.” – (Accessed June 2021) |
Pennsylvania | No. No relevant policy or statue reference found. |
Rhode Island | Yes, bill passed July 2021. “(2) All such medically necessary and clinically appropriate telemedicine services delivered by in-network primary care providers, registered dietitian nutritionists, and behavioral health providers shall be reimbursed at rates not lower than services delivered by the same provider through in-person methods.” – (Accessed July 2021) |
South Carolina | No. No relevant policy or statue reference found. |
South Dakota | No, coverage parity only. “No health insurer may exclude a service for coverage solely because the service is provided through telehealth and not provided through in-person consultation or contact between a health care professional and a patient. Health care services delivered by telehealth must be appropriate and delivered in accordance with applicable law and generally accepted health care practices and standards prevailing at the time the health care services are provided, including rules adopted by the appropriate professional licensing board having oversight of the health care professional providing the health care services. Health insurers are not required to provide coverage for health care services that are not medically necessary.” – (Accessed May 2021) |
Tennessee | No, coverage parity only. “(e) A health insurance entity shall provide coverage for healthcare services provided during a provider-based telemedicine encounter in a manner that is consistent with what the health insurance policy or contract provides for in-person encounters for the same service, and shall reimburse for healthcare services provided during a provider-based telemedicine encounter without distinction or consideration of the geographic location, or any federal, state, or local designation or classification of the geographic area where the patient is located. (f) This section does not require a health insurance entity to pay total reimbursement for a provider-based telemedicine encounter in an amount that exceeds the amount that would be paid for the same service provided by a healthcare services provider for an in-person encounter. (g) (4) This section does not require a health insurance entity to reimburse a healthcare services provider for healthcare services delivered by means of provider-based telemedicine if the applicable health insurance policy would not reimburse that healthcare services provider if the same healthcare services had been delivered by in-person means.” – (Accessed May 2021) |
Texas | No, coverage parity only. “(a) A health benefit plan: (1) must provide coverage for a covered health care service or procedure delivered by a preferred or contracted health professional to a covered patient as a telemedicine medical service or telehealth service on the same basis and to the same extent that the plan provides coverage for the service or procedure in an in-person setting; and (2) may not: (A) exclude from coverage a covered health care service or procedure delivered by a preferred or contracted health professional to a covered patient as a telemedicine medical service or a telehealth service solely because the covered health care service or procedure is not provided through an in-person consultation” – (Accessed May 2021) |
Utah | Yes. “(2) Notwithstanding the provisions of Section 31A-22-618.5, a health benefit plan offered in the individual market, the small group market, or the large group market shall: (a) provide coverage for: (i) telemedicine services that are covered by Medicare; and (ii) treatment of a mental health condition through telemedicine services if: (A) the health benefit plan provides coverage for the treatment of the mental health condition through in-person services; and (B) the health benefit plan determines treatment of the mental health condition through telemedicine services meets the appropriate standard of care; and (b) reimburse a network provider that provides the telemedicine services described in Subsection (2)(a) at a negotiated commercially reasonable rate.” – (Accessed May 2021) |
Vermont | Yes. “(a)(1) All health insurance plans in this State shall provide coverage for health care services and dental services delivered through telemedicine by a health care provider at a distant site to a patient at an originating site to the same extent that the plan would cover the services if they were provided through in-person consultation. [Subdivision (a)(2) repealed effective January 1, 2026.] (2)(A) A health insurance plan shall provide the same reimbursement rate for services billed using equivalent procedure codes and modifiers, subject to the terms of the health insurance plan and provider contract, regardless of whether the service was provided through an in-person visit with the health care provider or through telemedicine.” – (Accessed February 2021) “2020 Acts and Resolves No. 91, Sec. 27 (repealing 8 V.S.A. § 4100k(a)(2), telemedicine reimbursement parity, on January 1, 2026) is repealed.” – (Accessed May 2024) |
Virginia | Yes. “An insurer, corporation, or health maintenance organization shall not be required to reimburse the treating provider or the consulting provider for technical fees or costs for the provision of telemedicine services; however, such insurer, corporation, or health maintenance organization shall reimburse the treating provider or the consulting provider for the diagnosis, consultation, or treatment of the insured delivered through telemedicine services on the same basis that the insurer, corporation, or health maintenance organization is responsible for coverage for the provision of the same service through face-to-face consultation or contact.” (Accessed April 2022) |
Washington | Yes. “(b)(i) Except as provided in (b)(ii) of this subsection, for health plans issued or renewed on or after January 1, 2021, a health carrier shall reimburse a provider for a health care service provided to a covered person through telemedicine at the same rate as if the health care service was provided in person by the provider. (ii) Hospitals, hospital systems, telemedicine companies, and provider groups consisting of eleven or more providers may elect to negotiate a reimbursement rate for telemedicine services that differs from the reimbursement rate for in-person services.” – WA & as amended by (Accessed May 2021) |
West Virginia | Yes, for established patients and patients in acute care facilities. “The plan shall provide reimbursement for a telehealth service at a rate negotiated between the provider and the insurance company for virtual telehealth encounters. The plan shall provide reimbursement for a telehealth service for an established patient, or care rendered on a consulting basis to a patient located in an acute care facility, whether inpatient or outpatient, on the same basis and at the same rate under a contract, plan, agreement, or policy as if the service is provided through an in-person encounter … .” – (Accessed March 2022) |
Wisconsin | No. No relevant policy or statue reference found. |
Wyoming | No. No relevant policy or statue reference found. |
About Manatt Health
Manatt Health integrates legal and consulting expertise to better serve the complex needs of clients across the health care system.
Combining legal excellence, firsthand experience in shaping public policy, sophisticated strategy insight, and deep analytic capabilities, we provide uniquely valuable professional services to the full range of health industry players.
Our diverse team of more than 160 attorneys and consultants from Manatt, Phelps & Phillips, LLP, and its consulting subsidiary, Manatt Health Strategies, LLC, is passionate about helping our clients advance their business interests, fulfill their missions, and lead health care into the future. For more information, visit .
About Manatt on Health
provides in-depth insights and analysis focused on the legal, policy and market developments that matter to you, keeping you ahead of the trends shaping our evolving health ecosystem. Available by subscription, Manatt on Health provides a personalized, user-friendly experience that gives you easy access to Manatt Health’s industry- leading thought leadership. Manatt on Health serves a diverse group of industry stakeholders, including five of the top 10 life sciences companies, as well as leading providers, health plans, hospitals, health systems, state governments, and health care trade associations and foundations. For more information, contact Barret Jefferds at
